Overview about Evidence-based Practice (EBP)
When evidence-based practice was first introduced in nursing?
The earliest demonstrations of evidence-based practice in nursing date back to the 1850s when Florence Nightingale’s book Notes on Nursing outlined the framework for evidence-based nursing practice as we know it today. The term evidence-based practice made its appearance in literature in 1996 and was defined as “the conscientious, explicit, and judicious use of current best evidence in making decisions about the care of individual patients.” (Sackett DL, Rosenberg WM, Gray JA, Haynes RB, Richardson WS. Evidence-based medicine: what it is and what it isn’t. BMJ. 1996;312(7023):71–72) In her 1999 publication, “About Evidence-Based Nursing Practice” in Nursing Management, Marjorie Beyers discussed the requirements and benefits of implementing an evidence-based practice nursing model.
Who introduced evidence-based practice in nursing?
Several sources have been credited with introducing evidence-based practice in nursing. One source is Professor Archie Cochrane, an epidemiologist from the United Kingdom, whose research studies indicated that practices based on evidence instead of traditional care trends, resulted in improved outcomes for patients and staff. Additionally, Florence Nightingale’s endeavors in the 1800s and Gordon Guyatt, who is known as one of the earliest advocates for evidence-based medicine, have impacted EBP and are credited with some form of theory related to evidence-based practices in nursing.
What is the difference between evidence-based practice in nursing and research in nursing?
There is some misconception that evidence-based practice in nursing and research in nursing are the same. However, while there are similarities, there are some distinct, fundamental differences. The main difference between EBP in nursing and nursing research is their purpose.
The fundamental purpose of evidence-based practice in nursing is to use the best evidence available to make informed decisions about patient care. Research in nursing is used to validate existing nursing knowledge based on theory and generate new knowledge to promote better nursing practices and promote favorable patient outcomes. While most of the best evidence used in nursing practice stems from nursing research, EBP in nursing goes further to translate evidence from research and apply it to clinical nursing practices.
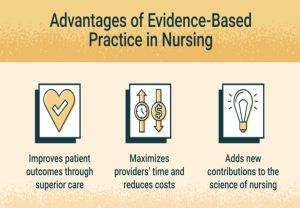
What are the benefits of evidence-based practice in nursing?
The importance of evidence-based practice in nursing is undeniable, especially as we continue to gather new research and test theories related to patient care. EBP in nursing aids nurses in pinpointing strategies to patient care and has become a vital component of high-quality patient care. Below, you will find the top five benefits of evidence-based nursing practices as they apply to patients, nurses, and healthcare organizations.
Top 5 Benefits to the Patient
- Evidence-based practice in nursing promotes positive patient outcomes by supporting a shared decision-making approach between nurses and patients.
- Reduced Risk of Hospital-Acquired Infections: One of the most common, yet preventable problems associated with hospital admissions is the risk of hospital-acquired infections. When nurses implement proven, evidence-based infection control measures, the risk of patients developing HAIs is greatly reduced.
- EBP in nursing allows nurses to involve patients in their care planning, promoting patient autonomy, which is a patient right.
- Another benefit of evidence-based practice in nursing is that it prompts nurses to alter methods of care if the current care plan contradicts best evidence-based practices, contributing to improved patient care.
- Reduced Cost of Healthcare: Because evidence-based practices in nursing aim to prevent complications or unforeseen patient issues, they are instrumental in reducing healthcare costs.
Top 5 Benefits to the Nurse
- Evidence-based practice in nursing provides nurses with scientifically supported research to help them make well-educated decisions.
- EBP in nursing helps nurses stay up-to-date about new nursing interventions and protocols used in patient care.
- Evidence-based practice for nurses enhances critical thinking among nurses.
- Another benefit of evidence-based practices in nursing is that they promote strong decision-making skills
- Because evidence-based practices are based on research, the use of EBP encourages lifelong learning.
Top 5 Benefits to the HealthCare Organization
- EBP in nursing helps promote consistent care to patients based on evidence-driven research findings.
- With the use of evidence-based practice in nursing, more favorable patient outcomes are achieved, resulting in increased patient satisfaction. Patient satisfaction scores are important to healthcare organizations because they impact reimbursement from financial institutions.
- When implemented properly, evidence-based practices in nursing can reduce the demand for healthcare resources, making it possible to allocate resources where they will be most effective.
- Evidence-based practices in nursing help reduce healthcare costs by utilizing relevant research to determine the most appropriate and cost-effective treatment options for patients.
- Healthcare organizations benefit from evidence-based nursing interventions by having knowledgeable nurses, capable of understanding and implementing the best methods of patient care for clients.
Definition and Components of Evidence-based Practice (EBP)
- It involves the use of published research in addition to one’s clinical expertise and patient preferences.
- EBP is a core component of clinical practice across all levels of nursing education.
- Nurses practicing across clinical settings are at the forefront of healthcare. These nurses serve a critical role in bridging the gap between practice and theory.
- The consistent application and integration of EBP into all levels of nursing practice leads to high-quality health care, improved patient outcomes, and healthcare cost savings.
- To increase the use of EBP, nurses must develop a strong foundation in the EBP process.
- EBP ensures:
-
- Efficacy: (the ability to reach a desired result under ideal condition).
- Efficiency: (the achievement of a desired result with a minimum of expense, time, and effort).
- Effectiveness: (the ability to produce the desired result under usual condition).
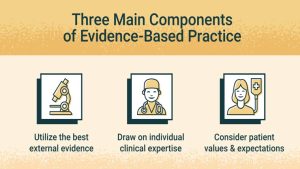
Best Scientific Evidence
- The best scientific evidence is the results of the best available scientific studies. It is used to find out which treatments, diagnostic methods, or ways of predicting a patient outcome work best.
- Scientists carefully design studies to measure how well things such as treatment and diagnostic tests work.
- Scientific evidence can provide a higher-level view than expert opinions or objective data to help inform healthcare decisions, and is one of the important pieces of evidence-based practice.

Clinical Expertise
- It is the provider’s judgment about what works best in similar patients or in similar situations.
- Health is complex and there is not high-quality research on every topic.
- Through years of practice, healthcare providers develop clinical expertise that guides patient care decisions.
- This clinical judgment is essential for applying evidence-based practice.

Patient’s Preferences and Values
- Patients’ or clients’ needs and values are what is important for the patient or client and what healthcare options best match those values.
- There are many conditions where patient needs and preferences are important factors in choosing the right treatment or screening option.
- Cost of care, quality of life, and personal beliefs are all important considerations.
- Patients should be partners in their care and help decide what type of healthcare is best for them.
- Evidence-based practice recognizes that patient values are essential in determining care.
Practical problems and EBP solutions
- Problem: Patient care questions remain unanswered. Studies have shown that the frequency of questions raised by clinicians ranges from .16 to 1.85 per patient seen. Due to lack of time, lack of information resources, and weak search skills, clinicians are only seeking answers to 50% of those questions.
- EBP Solution: Evidence-based practice tools and methods make it faster and easier to find the best evidence, especially at the point of care where it matters most. This means that more questions can be answered, health care can become more evidence-based, and outcomes potentially improved.
- Problem: Healthcare literature, with clinically applicable findings, is published at a rate that is impossible for individual clinicians to keep up with. A 2010 study indicated that there were over seventy-five clinical trials and eleven systematic reviews published every day in medicine. At ten minutes an article, it would take over fourteen hours every day to read them all.
- EBP Solution: Systematic reviews, evidence-based practice summaries, clinical practice guidelines, and peer-reviewed article lists are all examples of EBP tools that help to tame this flood of information by summarizing the best information.
- Critical appraisal: Make it easier to look at an article and be able to quickly determine its strengths and weaknesses and its use for patient care. A core element of EBP is the focus on patient-oriented outcomes such as death, disability, and discomfort rather than disease-oriented outcomes such as lab results.
- EBP tools and methods: Can help you to easily separate the best, clinically relevant and patient-oriented evidence from the rest.
- Problem: It can take more than a decade for clinical research to be fully integrated into everyday practice. Even once evidence is widespread, providers still make decisions based on habit rather than evidence.
- EBP Solution: By making good evidence easier to find and appraise, EBP can reduce this delay and provide better support for changing care.
