Session (8)
Management of change
Evidence-based practice (EBP) is dependent on more than just finding evidence. Introducing EBP involves change. Various barriers and enablers might be encountered when attempting to change practice. Barriers and enablers to change can occur across different levels of healthcare and at different times.
Identify the barriers to change
When implementing any new policy or guidance, it is essential to identify the gap between recommended practice and current practice (baseline assessment). Ideally, this assessment will also help to identify the potential and actual barriers to change, allowing you to pinpoint the practical actions needed to implement the change along with the groups of professionals who are key in bridging this gap.
Consequently, to develop a successful strategy for change, you need to: –
- Understand the types of barriers faced in healthcare.
- Identify the barriers to change in your organization.
- Overcome these barriers, and highlights potential levers.
- Encourage changes in behavior and ultimately implement guidance.
Barriers and enablers to evidence-based practice
- The change itself
- Ability to access and assess evidence
- Local environment
- Workplace culture
- Clinical skills
- Patient values, concerns and expectation
- Financial and human resources
A: The change itself
- Likely to save time, energy, and resources (Feasibility)
- Published evidence of proven benefit (Credibility)
- Has worked in other environments (Accessibility)
- Able to be incorporated into existing systems (Attractiveness)
B: Ability to access and assess evidence
The ability to locate and appraise appropriate information to answer their clinical questions.
C: Local Environment
- Access to electronic clinical information,
- The development of local policy.
- The suitability of the physical environment.
D: Workplace culture
- Support for change, effective communication, staff attitudes and well-developed change management skills influence the healthcare professionals’ desire, motivation and ability to make changes.
- Other professionals may not believe that recommendations reflect the evidence or that they will achieve better patient outcomes.
- A person’s belief in his or her own ability to adopt a new behavior also has an impact on whether a change is implemented.
E: Financial and human resources
- Cost is always a consideration in any health service. New treatments may not be introduced for some time due to lack of funds or shortage of necessary resources or personnel.
- New equipment might be needed in order to enable new guidance to be followed.
F: Clinical skills
- Change may be delayed while new skills and knowledge are developed.
- Healthcare professionals may need training to ensure they have the skills to deliver best practice.
- They may need the time to learn new skills and practice them.
- Support from peers or mentoring might be needed.
G: Patient values, concerns and expectations
Patients may expect and request improved services or specific treatments because of increased knowledge about evidence-based healthcare. Patients may also refuse recommended treatments for social, cultural, or religious reasons.
Methods to identify the barriers to change
Your choice of method will be guided by local circumstances, including the numbers of professionals involved and the time and resources available. In some situations, more than one approach may be needed.
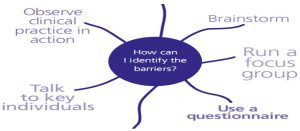
- Talk to key individuals
- It enables ideas to be explored in an iterative fashion.
- Detailed information can be obtained.
- It is quick and inexpensive.
There may be some disadvantages, for example:
- It relies heavily on the key individual(s).
- The responses may be subject to bias.
- It may be difficult to find the right person (or people) to talk to.
- Additional corroboration may be needed.
- Observe clinical practice in action
- It enables detailed analysis of current behaviors in context.
- It eliminates reporting bias.
- It can provide a useful method for monitoring progress, if repeated on a regular basis.
There may be some disadvantages, for example:
- It can be difficult to gain consent from the people you want to observe.
- Peoples’ behavior can alter when they know they are being watched.
- A skilled observer is needed to minimize influence on the person being observed.
- Methods of data collection need careful consideration.
- Use a questionnaire
- Questionnaire is a good way of exploring the knowledge, beliefs, attitudes and behavior of a group of geographically dispersed healthcare professionals.
- It allows rapid collection of relatively large amounts of data from a large number of people.
- It enables statistical analysis of standardized data.
- It provides the opportunity to highlight the need for change through communication of the results.
- It is relatively inexpensive.
There may be some disadvantages, for example:
- Significant time is needed to develop good questions.
- It is not possible to ask follow-up questions.
- The response rate may be poor and may be biased towards high performers.
- The nature of self-reporting means it can be inaccurate.
- Brainstorming is a way of developing creative solutions to problems.
- It can be done informally in small groups or as part of a focus group.
- It is fast and easy to do.
- It generates lots of ideas.
- It helps engage people in the process of change.
There may be some disadvantages, for example:
- It needs a skilled facilitator.
- More vocal members of the group may dominate the discussion.
- Organizing a session among a group of healthcare professionals can be difficult because of their clinical commitments.
- Run a focus group
- Focus groups are a powerful means of evaluating current practice and testing new ideas.
- They comprise a facilitated discussion or interview involving a group of 6–10 people.
- Open questions are posed by the facilitator, who then encourages the group to discuss their experiences and thoughts, and reflect on the views of others.
- It enables a representative group of people to share ideas
- It allows a wide range of in-depth information to be obtained
- It encourages new ideas and perspectives
- it helps get people engaged in the change process
- It is relatively quick and easy to perform.
There may be some disadvantages, for example:
- A skilled facilitator is needed to ensure everyone is able to express their views.
- It can be difficult to find a suitable time for everyone to attend.
- Incentives may need to be offered to encourage attendance.
- Analysis can be time consuming.
- Careful planning and analysis are needed.
Overcome the barriers to change
There is no one method to overcome all the different barriers; different approaches will be effective for different people and different situations. These methods can be used on their own or together; combining methods may have a bigger impact on change.

- Educational materials
Booklets, leaflets, journal supplements, CD-ROMs, videos and DVDs, online tools and computer programs are often used to inform healthcare professionals about the latest developments in their field.
For example: At NICE a ‘quick reference guide’, summaries our recommendations, designed especially for the healthcare professionals upon whom it impacts. This document alerts the reader to key changes in practice and provides a resource that can be referred to repeatedly.
- Educational meetings
Conferences, workshops, training courses and lectures are often used to educate healthcare professionals about the latest developments in their field.
These meetings can be divided into two categories:
- Large-scale meetings, such as lectures and conferences where the audience is largely passive.
- Small-scale meetings, such as interactive workshops and training courses where the participants take a more active role in learning.
- Educational outreach visits
- Also known as academic detailing.
- They were originally used by the pharmaceutical industry to influence the prescribing behavior of doctors.
- Trained individuals visit healthcare professionals in their own practice and offer information, support and instruction in line with current best practice.
- Opinion leaders
- Opinion leaders use their influence to motivate and inspire healthcare professionals to achieve the best possible care for patients.
- They are well respected among their peers and act as role models for junior colleagues.
- They can make a positive difference in a variety of ways, from providing a signature for a letter accompanying the guidance, to delivering speeches, writing articles in influential journals or undertaking outreach visits.
- Clinical audit and feedback
- Clinical audit and feedback involves retrospective reporting of information to individuals or organizations about their practice as part of a drive to improve quality.
- Data are collected from actual practice to provide insight into particular aspects of care, through either:
- Internal audit, where healthcare professionals are involved in data collection,
- External audit, where others collect and collate the information.
- Feedback may be on outcomes of care, costs or other elements of clinical performance, and may also include a comparison against peers.
- Reminder systems
- Reminders and computer-aided decision-support systems aim to provide healthcare professionals with specific information, when they need it.
- These prompts are designed to reflect best practice and remind healthcare professionals to take or avoid a certain action.
- Reminder stickers on medical notes and computer-aided decision-support systems all enable quick access to patient-specific best practice during a consultation.
- Patient-mediated strategies
- Patient-mediated strategies focus on giving information to patients and the wider public.
- These strategies can help to change the behavior of healthcare professionals in a number of ways:
- Equipped with knowledge about the latest evidence-based practice,
- Patients are more able to influence decisions made during consultations about their care.
- Patients are also more accepting of any changes to their care if they know that it is in line with the evidence.
- There is evidence that mass media campaigns work by educating both professionals and patients about changes in practice. Patients are also more likely to adhere to the treatment offered if they are well informed, which in turn helps to keep professionals motivated.