Session (2)
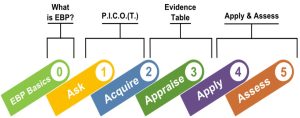
Process/Steps of Evidence-Based Practice
There are five steps to EBP:
- 0) Cultivate a spirit of inquiry,
- 1) Ask a clinical question,
- 2) Acquire information/evidence to answer the clinical question,
- 3) Appraise the evidence,
- 4) Apply (combine evidence with clinical experience and patient preferences),
- 5) Assess and disseminate the results.
The Process of Evidence-Based Practice
- Nurses and other members of the healthcare team often wonder why clinical practices are performed in a certain way or if those practices could be improved.
- Nurses are trained to think critically and apply this enhanced thought process to all aspects of patient care. This way of thinking often cultivates a spirit of inquiry, which is considered step 0 of EBP and leads to clinical questions.
Step 1: Ask PICOT question

- Developing a clinical question is the first step of the EBP process.
- Clinical questions must be formed in a subjectively and objectively measurable manner.
- One common method of developing a clinical question is the PICOT method.
- The acronym PICOT helps to clarify the clinical question, taking a broad idea and refining it into a more specific and narrow research question.
- Clinical questions that are broad and nonspecific can lead to false assumptions and may not be answerable or clearly define the problem.
- A good PICOT question must be specific enough to clearly define a problem, but broad enough to make finding evidence possible.
Importance of formulating clinical questions using (PICOT) model
- It helps to focus on the most relevant paper(s).
- It increases efficiency of search for the evidence.
- It helps you to set the desired outcomes.
- It can help identify useful key words for a search and will increase the chances of finding an appropriate answer to the question.
- Using PICO format helps you find a needle in a haystack of research information.
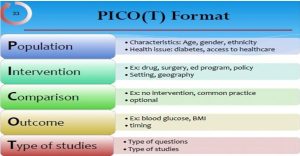
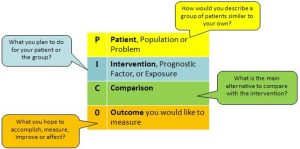
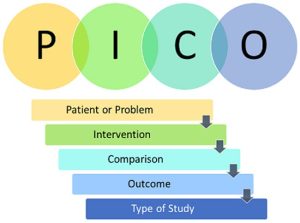
The components of a PICOT question:
- P: Problem, population, or patient
- I: Intervention, independent variable, or indicator
- C: Comparison
- O: Outcome or dependent variable
- T: Time frame
Template for Asking PICOT Questions
Among/Within/For/In ……P………, does/Can………I…… Compared to……C…….. affect……O……?
The following case scenario is an example of how a PICOT question is developed in the clinical setting.
Case Scenario (Population)
A wound care nurse working on a medical-surgical unit in a large hospital knows that pressure ulcers are a significant cost to the healthcare system and detrimental to patient health. The nurse recognizes that the incidence of all types of pressure ulcers is increasing on her unit. After a chart review, she realizes that nurses are not documenting pressure ulcers that are present on admission, are not measuring and staging the wounds consistently, and are not formulating a proper treatment plan based on accurate staging. The nurse formulates a clinical question to address the inconsistencies in documentation, staging, and treatment of the pressure ulcers in (P) medical-surgical patients in an acute care setting.
- The (P) in the PICOT describes the problem, population, or patient, along with pertinent characteristics, demographics, or health issues.
- The rest of the PICOT question defines the intervention that will be implemented,
- How the outcome will be measured or compared,
- What outcome is expected, and
- Time frame needed to gather the necessary data.
Intervention:
The wound nurse, nurse manager, and nurse educator on the medical-surgical unit form a task force to investigate the pressure ulcer problem in their patient population. The task force reviews the evidence-based literature base and then performs an appraisal of the research available. They find a great deal of quality research that indicates a lack of education on pressure wound staging and assessment is a common inhibitor to proper prevention and treatment.
- Integrating the EBP research gathered, the wound nurse creates an annual educational activity and corresponding competency based on the National Pressure Ulcer Advisory Panel’s prevention protocol. The nurses on the unit will be required to take the training program and competency on an annual basis to confirm continued proficiency.
- The nurses are able to formulate their intervention, (I) implementation of educational material, and a yearly competency for pressure wound assessment and staging using the information acquired from the literature appraisal.
- The (I) in the PICOT question defines intervention, independent variable, or indicator.Examples of these include medications, surgery, educational programs, or policy changes.
Comparison: Comparison is the (C) component in the PICOT question.
The (C) will often include no intervention or the current or common practice.
- This component can be difficult to determine at times, and there are instances where the C can be omitted, especially if the study does not have a control group, comparison group, or alternate treatment option to compare.
- In the example of the medical-surgical unit, there will not be a comparison or alternative intervention. The study would have to leave half of the nurses out of the competency for the specified amount of time to create a control group.
- The wound nurse chooses to compare the rate of pressure wounds after the intervention to the prior rates with the previous treatment.
- So, the PICOT would say (I) how does the implementation of a yearly competency for pressure wound assessment and staging (C) compare to no yearly competency for pressure wound assessment and staging?
- Outcome and Time:
The expected outcome for the medical-surgical unit is a decrease in the incidence of HAPU. The outcome for the PICOT question would state (O) affect HAPU rates. The nurses elect to continue with quarterly measurements of HAPU incidence. Since measurements are taken quarterly, the time will state (T) within 3 months.
- Taking each unit of the PICOT question from the case scenario and combining each section results in the following question:
“For (P) medical-surgical patients in an acute care setting (I) how does the implementation of a yearly competency for pressure wound assessment and staging (C) compare to no yearly competency for pressure wound assessment and staging (O) and affect HAPU rates (T) within 3 months?”
Formulating the Question
There are generally two types of questions: background questions and foreground questions.
Background Questions
- Background questions ask about general knowledge and usually consist of two parts: the root question (what, where, when, why or how); and a specific disease or treatment. Some examples of background questions include:
- What are the clinical signs of measles infection?
- What are the potential side effects of NSAIDs?
- What warming methods are used to treat hypothermia?
Foreground Questions
- Foreground questions are focused questions that help us make clinical or situational decisions. They are more complex and include specific information about patients, interventions, and outcomes. Most of the questions we will focus on in this tutorial are foreground questions, and we will use the PICO framework to structure a well-built PICO question.
- What is a well-built question, and why is it important?
- When you are presented with a scenario or patient case, there is usually a flood of details to digest. To effectively search for the best evidence, you first need to decide which details are important.
Here are some details that you might find important:
- Who is the patient, population, or problem?
- Is their medical or social history important?
- What characteristics of the patient matter?
- Are certain signs and symptoms relevant?
- Identifying the important details and forming a succinct clinical question will make it easier for you to search for evidence later in Step 2.
PICO
- It is a state of mind. The PICO framework is a systematic way to identify important concepts in a case, and formulate a question for searching.
- However, PICO is very relevant to patient and treatment scenarios, and some questions do not fit perfectly into the PICO format. For example, you may not have a specific comparison intervention, or may have multiple outcomes you are interested in. Do not worry about this!
- The goal of PICO is to focus your topic, and your question can always be refined and changed.
- Remember, no matter what type of resource you will ultimately use to look for answers, you should always start by applying PICO to your question so you can think about it strategically.
PICO examples
Here are two example clinical scenarios where the most important elements of the scenario have been identified using the PICO framework.
Example 1
Tom is 55 years old and has smoked one pack of cigarettes a day for the last 30 years. He is ready to quit, and is wondering about his options. He has heard of a medication called bupropion, but is also familiar with nicotine replacement therapy options such as patches, lozenges, and gum. Tom wants to know which option will work best to help him quit and abstain from smoking again in the future.
- Patient/problem/population: mid-50s male with a 30 pack-year history of smoking.
- Intervention: bupropion.
- Comparison intervention: nicotine replacement therapy.
- Outcome: long-term abstinence from smoking.
Example 2
Janet is 42 years old and just had her first mammogram. She does not have a history of breast cancer in her family, and she has heard from her friends that she does not need to have a mammogram every year, only every three years because of new guidelines. She wants to know if she has to come back every year for a mammogram, or if she can make an appointment every three years.
- Patient/problem/population: woman in her 40s with no family history of breast cancer.
- Intervention: mammograms every three years.
- Comparison: yearly mammograms.
- Outcome: early detection of breast cancer.
Framing good questions
- Once you have identified the core concepts of your topic using the PICO framework, how do you translate them into a question?
Describe the subject of the question.
- It may be helpful to phrase the question in this form: “How would I describe a group of patients similar to this one? What are the relevant characteristics?”
Define which intervention you are considering for the specific patient or population.
- It is sometimes helpful to name a second intervention with which to compare the first.
- This might be another treatment, placebo, or ‘usual care.’
- For example, diagnosis via a traditional X-ray is often compared to diagnosis with an MRI. However, it is not always necessary to include a comparison.
Define the type of outcome you wish to assess.
- There are many possible outcomes. Try to focus on patient-oriented outcomes like death, disability or discomfort. These could include mortality, disease progression, results of a diagnosis test, confidence/anxiety, cost effectiveness and more.
Example 1
- Patient/problem/population: mid-50s male with a 30 pack-year history of smoking
- Intervention: bupropion
- Comparison intervention: nicotine replacement therapy
- Outcome: long-term abstinence from smoking
A well-built clinical question for these PICO elements would be:
In a 55-year-old man, would the administration of bupropion therapy versus nicotine replacement therapy lead to long-term abstinence from smoking?
Example 2
- Patient/problem/population: woman in her 40s with no family history of breast cancer
- Intervention: mammograms every three years
- Comparison: yearly mammograms
- Outcome: early detection of breast cancer
A well-built clinical question for these PICO elements would be:
In a 42-year-old woman with no family history of breast cancer, are mammograms every three years as effective in detecting breast cancer as yearly mammograms?
Here are some other examples of clinical questions. Even though we do not have the example clinical scenario or the PICO frameworks for the below questions, you can easily tell what the most important elements of the patient scenarios are:
- In a 50-year-old man with low back pain, is physical therapy as effective at relieving pain as surgery?
- In a 34-year-old woman with chronic cold sores, does taking zinc work help to prevent cold sores?